Cell therapies
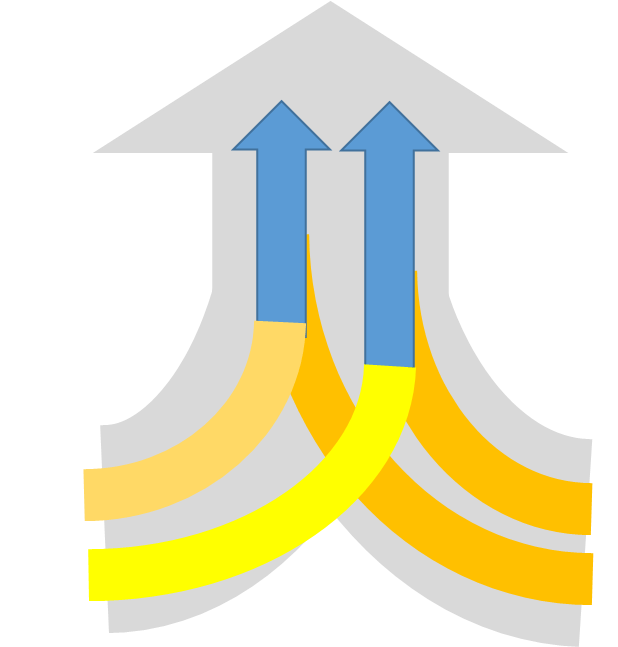
While gene therapy approaches aim to treat existing cells within the retina, cell therapy strategies aim at adding new cells to the tissue. Particularly regarding the replacement of RPE cells and photoreceptors via transplantation, the research field has dramatically progressed within the past decade resulting in the first clinical trials for cell therapy in Stargardt disesase and age-related macular degeneration (AMD) with RPE cells derived from pluripotent stem cells (MacLaren et al. 2016).
Though first attempts in cell therapy for the replacement of photoreceptors date back to the late 1980ies, important pre-clinical studies during the last years provide evidence for the feasibility of cell-based retinal repair by photoreceptor transplantation. It was shown that young post-mitotic photoreceptors precursors rather than proliferating retinal progenitor cells showed long-term survival and maturation following transplantation into the adult degenerated mouse retina (MacLaren et al. 2006; Bartsch et al. 2008) culminating in functional improvements by rod transplantation in mouse models of RP (Pearson et al. 2013) and daylight vision repair by donor cone-like photoreceptors grafted into a cone degeneration model (Santos-Ferreira et al. 2015). Additionally, technologies for the enrichment of donor cells based on photoreceptor-specific fluorescent donor lines (MacLaren et al. 2006) or cell surface markers using flow cytometry (Lakowski et al. 2011) or magnetic activated cell sorting (MACS; Eberle et al. 2011) allowed significant improvements in transplantation outcomes. However, though MACS might represent a method usable under GMP conditions adaptable for clinical applications, marker-free purification approaches might be ideal circumventing potential side effects by antibody mediated sorting methods.
With the establishment of new cell therapy techniques to generate
in vitro expandable human pluripotent stem cells and their directed differentiation towards a retinal fate, a major roadblock towards photoreceptor/RPE cell therapeutic approaches was overcome as donor cells can now be generated in principle in unlimited quantity
in vitro . Particularly the establishment and optimization of
3D retina organoid culture techniques (Eiraku et al. 2011; Völkner et al. 2016) now allows the generation of sufficient amounts of photoreceptors from mouse and human PSCs for transplantation approaches (Gonzalez-Cordero et al. 2013; Decembrini et al. 2014; Santos-Ferreira et al. 2016). However, knowledge about transplantable PSC-derived human photoreceptors is still limited particularly with regard to the optimal ontogenetic stage for successful transplantation and, importantly, their potential maturation and functionality to repair visual impairment.
The main questions of the cell therapy research projects in the SPP 2127:
- How can we best obtain, culture and differentiate iPSCs in order to have optimally prepared retinal cells for transplantation?
- Can human iPSC-derived photoreceptors functionally integrate into the degenerated retina?
- Do 3D retinal cultures (i.e. organoids) represent a new potent tool in disease-modelling?
- Can we reliable modify the genome in iPSCs in a way that autologous re-implantation of differentiated retinal cells becomes a safe approach?